My husband, Andrew, and I felt truly blessed when we conceived right when we were ready. The pregnancy had been smooth and uneventful—normal, healthy, and full of anticipation—until our 20-week sonogram. I remember the joy as we settled into the room, seeing our baby for the first time on screen. We learned we were having a daughter, and we had already chosen a name: Sloane Eloise. It felt like pure bliss knowing our little girl was growing inside of me, already bringing so much love into our lives.
During the sonogram, I noticed the sonographer repeatedly focusing on Sloane’s left arm, but I didn’t think much of it at first. Later, when we met with our OB, her words brought a mix of worry and uncertainty: our sweet daughter appeared to have an underdeveloped left arm. My OB, with her compassion and patience, guided us gently, explaining that we would need a level II sonogram at Maternal Fetal Medicine (MFM) to understand more. We thanked her and headed home, the drive heavy with emotion and uncertainty.

I cried endlessly on the way home. I felt like I had failed my daughter before she’d even arrived. Looking down at my left hand and my wedding ring, a symbol of love and unity, I couldn’t help but wonder where Sloane would ever wear hers. My mind raced with a long list of things I thought she might not be able to do. For hours, hopelessness and fear consumed me. But eventually, Andrew and I were able to talk through it. We realized Sloane was healthy, and that was what truly mattered. With that, our learning journey began.
Weeks later, at our MFM appointment, it was confirmed: Sloane was indeed missing part of her left arm. The exact endpoint couldn’t be determined, yet her overall health remained intact. We were then referred to the local children’s hospital to meet with Neonatology, and by this point, we were beginning to feel more prepared and empowered to raise a child with a limb difference.

Sitting in the waiting room for our Neonatology appointment, I saw a mother visiting her newborn, just a few days after surgery. Listening to her family and seeing her courage filled me with perspective. If this family could face challenges so bravely, so could we. Resources like Children’s Mercy Hospital and the Lucky Fin Club gave us hope for Sloane’s future. Still, one lingering uncertainty remained—how would I see her when she finally arrived?
At 33 weeks, a simple cold meant I worked from home and took doctor-approved medication. I don’t usually take medicine, so I was hyper-aware of every fetal movement—this vigilance became our blessing. Midway through the day, I noticed less movement than usual and called my OB, who directed us to the hospital birth center. Initially, we had planned to visit urgent care afterward, thinking it was just the cold acting up, but everything changed once we arrived at the hospital.
Connected to fetal monitors, we heard her heartbeat, and relief washed over us. Then, a nurse came to “buzz my stomach” to encourage movement. At first, nothing seemed out of the ordinary, but soon the nurse returned with concerning news: Sloane’s heartbeat wasn’t what they liked to see. A biophysical profile at MFM was immediately scheduled.
During what seemed like another routine sonogram, the results were devastating. Our daughter scored 2 out of 10 on her biophysical profile, with only points for amniotic fluid. Her brain was not symmetrical, and fluid was present. The doctor ended with words we could never forget: “This is her eviction notice.” Urgently, we returned to my room, and preparations for an emergency C-section began. Neonatologists explained what to expect—a large team in the room, potential resuscitation, possible transfer to the children’s hospital.

The delivery was intense and surreal. The cord was wrapped around Sloane’s neck, she didn’t cry, and her breathing required CPAP. Yet, in one magical moment, as the team carried her out for stabilization, they paused to let me see her. Our little Sloane Eloise opened her eyes ever so slightly, meeting mine for the first time. In that instant, every fear melted away.

Her first head ultrasound showed a perfectly healthy brain. After 30 days in the NICU, Sloane finally came home. Genetic testing confirmed her limb difference was not caused by Amniotic Band Syndrome or another genetic condition. While we continue to learn about her unique needs, Sloane’s health remains the most important factor as we grow our family.
From the very beginning, Sloane has thrived. She visits the Children’s Mercy Rehabilitation Clinic for limb-difference care, including PT, OT, and prosthetic evaluations. Before her first birthday, we began the prosthetic process—measurements, test sockets, fittings—helping her gain new skills while respecting her independence. She has embraced her prosthetic with confidence, using it daily with joy and curiosity.

At just 21 months old, Sloane has already participated in therapy to strengthen her core, fine motor skills, and prosthetic training. For her, therapy is play, and she has consistently met her goals. She uses her ‘little arm’ and chin to hold toys, her left foot to turn pages, and she’s been swimming and climbing for over a year. We encourage her to find her own path, letting her determine how to approach challenges, building independence, resilience, and self-confidence.

Through social media, we’ve connected with other families raising children with limb differences, sharing stories, guidance, and support. The journey has been transformative, showing us the strength, creativity, and spirit that children like Sloane bring to the world.

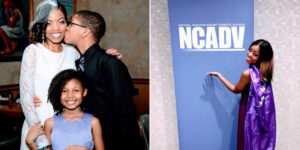
Sloane Eloise, whose name means “warrior,” truly lives up to it every day. She’s already teaching us lessons of courage, joy, and determination. And as we continue alongside her, we’re confident she will grow into a strong, independent young woman, educating and inspiring others through her journey.